therapist what to do if pacient is suicidal
We tell near every suicidal person to exercise information technology. It's role of most suicide prevention campaigns. When we don't have the answers, it'due south where we tell our loved ones they'll find them.
"Come across a therapist."
And yet suicide prevention experts say outside of psychiatrists, the bulk of mental health professionals have minimal to no formal training in how to effectively treat suicidal people.
Suicide-specific training is not ordinarily offered as part of college curriculums, optional postgraduate training opportunities are express, plush and time-consuming, and experts say some therapists may non be aware they fifty-fifty demand the educational activity.
"Any profession'south ethical standards require that you non care for a problem you don't know, and nevertheless every day thousands of untrained service providers encounter thousands of suicidal patients and perform uninformed interventions," said Paul Quinnett, a clinical psychologist and founder of the QPR Found, an organization that educates people on how to forbid suicide.
"People think if you send someone, a loved one, to a therapist, that therapist will exist skilled in how to address ... their risk for suicide. Nada could exist further from the truth."
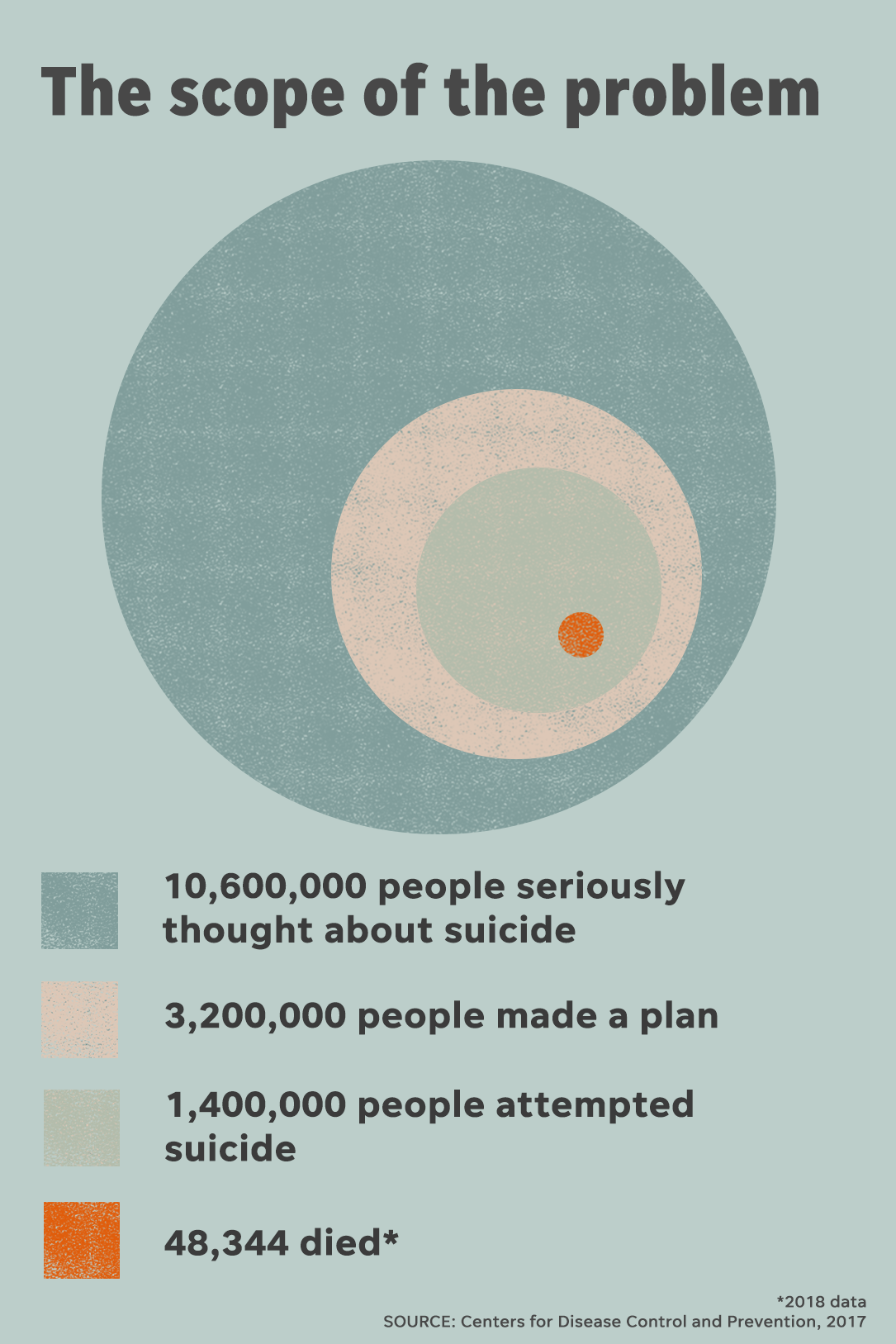
Numbers released in January from the U.S. Centers for Disease Command and Prevention show 48,344 people died by suicide in 2018, a small increase from the year before, though the ascent in deaths over time has been steady. Since 1999, the suicide rate has climbed 35%.
Suicide is the nation's 10th-leading cause of death, yet experts say training for mental health practitioners who care for suicidal patients – psychologists, social workers, marriage and family unit therapists, among others – is dangerously inadequate.
Many suicide prevention experts say combating suicide requires a holistic arroyo that includes communities, families, educators and religious leaders working together. Just society, they say, has placed the brunt of caring for suicidal people on a mental health workforce woefully underprepared to assistance them.
In Depth: Funding for suicide lags behind other top killers
In that location are no national standards that crave mental health professionals be trained in how to treat suicidal people, either during their instruction or their career. But nine states mandate training in suicide cess, handling and management for health professionals, according to the American Foundation for Suicide Prevention.
Having someone on your side that gets what you're going through, that can advocate for your needs, and that gives you the space to talk through your thoughts is a game-changer.
The American Psychological Association and the Quango on Social Work Didactics, which accredit graduate programs in psychology and social piece of work, have standards to gear up graduates to treat patients in crisis only practice not require specific competencies regarding suicide.
For its 2014 report on guidelines to amend training amongst the clinical workforce, the National Action Alliance for Suicide Prevention assessed the state of instruction by sending surveys to 443 academic institutions. Of those, 69 responded, and 70% said no specific training for suicide was provided.

A 2012 newspaper past the American Clan of Suicidology cites decades of studies that underscore the preparation gap, and experts say not much has changed in the concluding several years. Information technology found about half of psychology students receive formal classroom preparation on suicide during their graduate education. Only nigh 25% of social workers receive whatever suicide prevention grooming. Marriage and family unit therapists had even less. Most psychiatrists receive some instruction, but many experts agree it's bereft.
"When people ask me, 'Who should I meet?' the only thing I tin can say is 'See a psychiatrist if you tin,' considering ... they're supposed to cover that topic during the class of their grooming," Quinnett said. "You have some assurance that they know something most it. Only you can't say that for whatsoever other (mental health) profession, which is astounding to me."
Suicidal people accept a spectrum of experiences with therapy, some harmful, some lifesaving. Many people living with suicidal thoughts say when they plant the right clinician, someone who didn't overreact and who made an earnest endeavour to understand their pain, they felt less suicidal.
"Having someone on your side that gets what yous're going through, that can advocate for your needs, and that gives y'all the space to talk through your thoughts is a game-changer," said Whitcomb Terpening, a licensed clinical social worker and founder of The Semicolon Group, a therapy practice in Houston that works exclusively on suicide.
"They'll have your best interest in mind, not just to keep you lot live, merely to aid you find a life worth living."
When someone who's feeling suicidal opens upwards to a therapist, they do so expecting the person sitting across from them wants to understand their suffering. Merely Stacey Freedenthal, a suicide endeavour survivor and associate professor at the University of Denver Graduate School of Social Work, says a common feeling amidst therapists when they realize they're sitting across from a suicidal person is panic.
They worry the patient might try to kill themselves, could succeed and they may go sued or lose their license. Their reflex is to ship the patient to an emergency room.

"You've got this person who has taken weeks or months or more to work up the nerve to go to a professional and the professional is maxim, 'I tin can't help you, you accept to become somewhere else.' And that can be very harmful," Freedenthal said.
Inquiry shows emergency room visits and involuntary hospitalizations – triggered when a mental health professional believes someone is at imminent risk of killing themselves – tin can increase a person's risk of suicide.
Susan Stefan, a scholar and litigator on behalf of people with psychiatric disabilities, says that in many cases, an emergency room can exist the worst identify for a suicidal person.
"It's loud, it'south hurried, people are in a rush," she said. "In that location is no training, generally, for emergency physicians, or staff to deal with suicidal people. In many places, at that place's not much sympathy."
Even if a therapist doesn't overreact, that doesn't mean they know how to help. Freedenthal says she one time had a therapist who made her "promise" she would never do anything to hurt herself.
"That's groovy in principle, but I kind of wouldn't accept been going for assistance if it was that easy," she said.
I think we as a social club waste a lot of fourth dimension trying to stop people from killing themselves as opposed to exploring why they want to die in the first place.
Some therapists try to avoid the question of suicide birthday. Freedenthal says she always asks her students and even colleagues with decades of experience, "What is your fear almost asking someone if they're thinking of suicide?"
The most common answer: "That they'll say yes."
Some chronically suicidal people say they've been dropped by therapists who were unable to tolerate the intensity of their pain. Others say their clinicians were so fixated on predicting how likely they were to impale themselves, they didn't spend enough time listening to why they were injure or what they might need.
"A lot of people who say they're suicidal are trying to convey the depth of their despair," Stefan said. "I call back nosotros every bit a gild waste a lot of time trying to stop people from killing themselves as opposed to exploring why they want to die in the first place."
Back in the 90s, Quinnett was the clinical managing director at a mental health heart in Spokane, Washington. Ane twelvemonth, they lost 13 patients to suicide. When Quinnett reviewed the decease records, he realized his clinicians didn't know how to care for suicidal patients.
"They were practiced people. They were goodhearted. They were crushed when their patients died, simply they didn't even know how to ask the question, permit alone how to assess and manage the take a chance," he said.
Subsequently, Quinnett said he helped put together a comprehensive, mandatory training program on suicide. Once information technology was fully up and running, he said clinic deaths plummeted, to 1 or none a yr. Somewhen a new CEO took over and Quinnett said he decided to shutter the program over toll concerns. Quinnett said suicides started up again, and then he quit.
About all mental health professionals see suicidal patients at some point in their careers, experts say, yet only a pocket-size fraction seek out specialized training.
For those who exercise want it, it can be difficult to come past. Some of the best therapies aren't available for training at scale, and those that are require time and coin.
David Jobes is director of the Cosmic University of America'south Suicide Prevention Lab and created CAMS – Collaborative Cess and Management of Suicidality – widely regarded as ane of the about constructive approaches to treating suicidal patients. In the absence of training, Jobes said many clinicians spend most of their fourth dimension trying to care for a patient's underlying mental illness, rather than asking the person, "What makes you want to kill yourself?"
CDC data published in 2018 shows 54% of people who died past suicide had no known mental health condition.
CAMS, Jobes said, is a model that endeavors to understand the sources of people's suffering. Just very few people are trained, he said, and those who could benefit from it most have probably never heard of it.
Andrew Evans, president of CAMS-care, which trains practitioners on the CAMS approach, said concluding twelvemonth that the company trained about 5,000 mental wellness professionals in the U.S.
Unless you seek out on your own specialized training, and about people do not get this, it will become exquisitely painful for y'all and touch your well-existence.
"That's a drib in the bucket, because millions of people have suicidal thoughts," said Jobes, noting CDC data from 2017 that showed x.6 million American adults seriously thought about suicide.
Terpening, who works with suicidal patients, says that as long as preparation for mental wellness providers is voluntary, patients won't go the care they need.
"Everyone'southward told 'Reach out, there'south ever somebody to talk to.' But there isn't. Considering we're non trained in graduate schools, we're not trained in our clinical intern hours, we're non offered those kinds of opportunities," she said.
Lack of training, Terpening added, doesn't just get out practitioners sick-equipped, it leaves them afraid.
"Therapists desire to practice well, they just don't know how," she said. "Fear is born out of the unknown."
Many therapists are so frightened of treating suicidal people they'll screen out potential patients who they think may be at risk, Quinnett said. Clinicians also are agape of liability, though Stefan said the business organization is far less real than most mental wellness professionals think. Even if a grieving family sues, she said, most cases are not successful. Facts, all the same, are not e'er persuasive when the undesired outcome feels so catastrophic.
A survey of mental health providers in Colorado, which has one of the highest suicide rates in the nation, showed many exercise not think they need more training, but want it, according to a 2018 commodity in the Journal of Public Health Policy. It found providers reported being "generally pleased with their existing training and felt prepared to address suicide within their practice," though lxxx% supported mandating suicide-related standing education.

When confronted with the intensity of pain a suicidal person is feeling, some therapists notice themselves overwhelmed – wanting to help, fearing they're not capable, with stakes that feel enormously high.
"It is emotionally painful," said April Foreman, a clinician and board fellow member of the American Association of Suicidology. "Call back, you're a therapist because yous're emotionally sensitive, and and so we requite yous training to exist even more sensitive. Then we put yous in a room with someone who has the kind of pain and despair and behaviors that put them at hazard of dying.
Addressing suicide risk is not something yous can get trained in once and exist done. This is such a hard problem with such serious consequences that people are going to experience and be unprepared unless they are engaged in an ongoing mode.
"Unless yous seek out on your own specialized grooming, and most people do non get this, it will become exquisitely painful for y'all and touch your well-being."
Foreman says therapists practicing Dialectical Behavior Therapy, another highly constructive handling approach for severe suicide risk, are expected to accept a consultation team to aid manage stress and burnout.
"I volition tell yous, having lost patients to suicide, the consultation group is invaluable," she said.
Terpening says being able to talk with peers is a crucial part of her own self-care.
"The work can be isolating," she said, "so to be able to hear from other people is so helpful and so healing in means that a spin class never could be."
The issue of inadequate grooming has been documented for decades. In 2001, the National Strategy for Suicide Prevention said it was critical that "mental health personnel receive advisable graduate schoolhouse preparation on the bailiwick of suicide while preparing for their professions."
About 20 years afterward, experts say not enough has inverse. Anthony Pisani, associate professor of psychiatry and pediatrics at the Heart for the Written report and Prevention of Suicide at the University of Rochester, said it is essential the goal be met, and training must extend well beyond school.
"Addressing suicide risk is not something you can get trained in once and be done," he said. "This is such a difficult problem with such serious consequences that people are going to feel and be unprepared unless they are engaged in an ongoing way."
The American Clan of Suicidology report on gaps in mental health training fabricated several recommendations for improving care. It said accrediting organizations must include suicide-specific educational activity as function of their requirements so graduate programs have the training in their curriculum. Country licensing boards, it said, must require clinicians be competent in suicide handling.
And the report said government has a role to play, likewise, by requiring that health care systems receiving state or federal funds ensure their mental health professionals are trained in suicide risk detection, assessment, treatment and prevention.
Maybe, most importantly, experts say clinicians take to overcome their fear of non knowing with certainty who may alive or die.
"I get the fright – our licenses are our livelihood, nosotros need to be able to protect them," Terpening said. "Just we likewise have to exist able to see past the risk to do what'south right for our patients."
If yous or someone you know may be struggling with suicidal thoughts, y'all can phone call the U.S. National Suicide Prevention Lifeline at 800-273-TALK (8255) any time day or night, or chat online.
Crisis Text Line also provides free, 24/7, confidential support via text bulletin to people in crisis when they dial 741741.
The American Foundation for Suicide Prevention has resources to help if you lot need to find support for yourself or a loved ane.
Alia Due east. Dastagir is a recipient of a Rosalynn Carter fellowship for mental health journalism. Follow her on Twitter: @alia_e
Source: https://www.usatoday.com/in-depth/news/nation/2020/02/27/suicide-prevention-therapists-rarely-trained-treat-suicidal-people/4616734002/
0 Response to "therapist what to do if pacient is suicidal"
Post a Comment